A month ago there was an
article in Nature that summarized current efforts toward a vaccine for SARS-CoV-2. A total of 115 different projects were identified, 73 of them clearly moving forward. Not much specific is publicly known as yet about these different projects.
In this post, I want to start with some history about vaccination and a broad overview of vaccine strategies.
We'll take a look at specific projects for Covid in another write-up. I'm particularly interested to read up on modern approaches and what their chances of success are.
Variolation
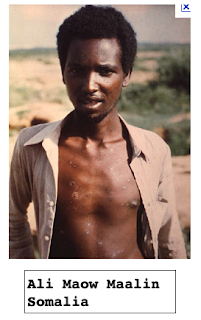
Smallpox has been a greatly feared viral disease that was eliminated from the earth in the 1970s. This guy is the last person to ever have smallpox.
(Except that the Russians kept samples, and apparently that lab had a fire recently).
Both Washington and Lincoln had smallpox, Washington as a young man when he visited the West Indies with his tuberculous brother Lawrence, and Lincoln about the time of the Gettysburg address.
Variolation involves taking pus from a smallpox patient and inoculating it to an uninfected person using a needle. Often the resulting case would be mild. It is an old
practice dating back at least to the 1500s if not before. It was brought to England in the early 18th century.
Maitland conducted an experimental variolation of six prisoners in Newgate Prison in London. In the experiment, six condemned prisoners were variolated and later exposed to smallpox with the promise of freedom if they survived. The experiment was a success, and soon variolation was drawing attention from the royal family, who helped promote the procedure throughout England.
The problem with variolation was that sometimes the smallpox that developed was severe. This led
Jenner to his famous development of the first vaccination (from the Latin vaccus, cow). Supposedly he noticed that milkmaids had clear complexions, completely lacking the smallpox scars that were quite common for other people. About 1798, he took samples of a virus related to smallpox, cowpox, and used that for inoculations with great success.
Vaccines
Classical vaccines are of three types. The first to be developed were inactivated proteins. These were made from protein (toxins) secreted by pathogenic bacteria as they are grown in culture. [
link] The toxins are collected from the supernatant, concentrated and inactivated with formaldehyde.
Diphtheria once was a major cause of illness and death among children. The United States recorded 206,000 cases of diphtheria in 1921, resulting in 15,520 deaths. Diphtheria death rates range from about 20% for those under age five and over age 40, to 5-10% for those aged 5-40 years. Death rates were likely higher before the 20th century. Diphtheria was the third leading cause of death in children in England and Wales in the 1930s.
Since the introduction of effective immunization, starting in the 1920s, diphtheria rates have dropped dramatically in the United States and other countries that vaccinate widely. Between 2004 and 2008, no cases of diphtheria were recorded in the United States.
There is a famous dog named Balto, part of a sled team that brought the diphtheria vaccine to Nome, Alaska during an outbreak in the 1920s. I'm not sure he'd be happy about it but Balto was stuffed and currently resides in a museum in Cleveland.
[Update: the
treatment for diphtheria was not a vaccine, but an "antitoxin", that is, antibodies to the toxin protein. Antitoxins are commonly made in large animals, especially horses. There is a vaccine, but that came later. ]
The other types of vaccine use the actual infectious agent. There is a vaccine for tuberculosis that is an attenuated strain of
Mycobacterium tuberculosis called BCG.
A vaccine against a virus like polio may be inactivated or alternatively, a live but attenuated virus. These vaccines depended originally on the development of mammalian cell culture and its use to produce virus in quantities large enough to immunize large numbers of people.
Inactivation is by treatment with chemicals (e.g. formaldehyde) or possibly UV. Attenuation means that the virus grows, but does not cause disease, either because it grows too slowly, or because it is unable to infect a particular tissue (poliovirus in the nervous system). Finding an attenuating mutant is a laborious process. In testing pathogenicity, there is no substitute for tests with live animals.
Besides tetanus, the first group of toxoid vaccines includes diphtheria. An example of the second is the Salk polio vaccine, and the third class includes many important vaccines including
-
Yellow fever
-
MMR (measles, mumps and rubella)
- Varicella (chickenpox)
- the oral (live) Sabin polio vaccine
- live (nasal spray) influenza vaccine
-
Smallpox
In the last 30 years or so, vaccines have been developed for
Streptococcus pneumoniae using its capsular polysaccharide, which may be chemically attached (conjugated) to a protein to make it more immunogenic. The capsule is important in preventing engulfment (phagocytosis) by cells of the immune system called neutrophils. Antibodies to the polysaccharide capsule allow phagocytosis and prevent disease.
Most viruses are first encountered by the host on mucosal surfaces in the mouth, the gut (digestive tract) or the airways (respiratory tract). In these environments a particular type of antibody called IgA is predominant.
Vaccine dogma holds that to produce strong immunity, a good IgA response is essential. The vaccine type which is best at achieving a good IgA response is thought to be an attenuated live virus vaccine, because it is the gift that keeps on giving. Continuous presence of the antigen drives antibody producing cells (B-cells) to switch to making IgA.
Three vaccines
IPV
The news of the success of the killed polio vaccine developed by
Jonas Salk was greeted with joy in 1955. This vaccine is called the Salk vaccine or IPV (inactivated poliovirus vaccine), and it's based on three wild, virulent reference strains: Mahoney (type 1 poliovirus), MEF-1 (type 2 poliovirus), and Saukett (type 3 poliovirus). The three viruses are grown in tissue culture (Vero cells, a type of monkey kidney cell), and then collected and inactivated with formaldehyde (formalin).
Salk's approach was widely criticized as dangerous, and indeed, in that same year a batch from the Cutter Laboratories in Berkeley, California was not properly inactivated and it
resulted in 200 cases of polio and 11 deaths.
OPV
A different vaccine using attenuated live virus was developed by
Albert Sabin, called the oral polio vaccine (OPV). It came into use around 1961. The OPV contains the three prevalent serotypes of poliovirus which have been passaged for many generations in tissue culture and accumulated mutations that do not interfere too much with growth in the gut, but prevent neurovirulence, growth in the nervous system. The individual components of the MMR vaccine were also developed in the 1960s.
It seems that the main reason the oral polio vaccine won out at that time was that the Salk vaccine is an injection, while the live virus is administered orally, often a drop or two on a sugar cube. Kids prefer the sugar cube. Also, sterile syringes are in short supply around the world. As an attenuated live virus, the Sabin vaccine is expected to be better at inducing a good IgA response. There is also evidence that the Sabin vaccine interferes with shedding of live poliovirus when they are both present, causing the live virus to die out.
The attenuated virus in the Sabin vaccine has been
sequenced (years later). Although there had been speculation about deletion mutations, apparently there are just a number of single nucleotide substitutions. Only a few of these are responsible for the attenuation phenotype in any given vaccine strain. [
review]
It happens rarely that the OPV causes authentic polio, a phenomenon called VAPP (vaccine-associated paralytic polio). The sequence of some VAPP strains shows reversion of the mutations in a one of the vaccine strains to change at least some of the attenuating mutations back to wild type. Also, it turns out that there are other naturally occurring viruses in the same family as poliovirus (Picornaviridae, for small RNA virus), which occur in nature and these may sometimes recombine with the live Sabin virus to give a recombinant that has recovered the ability to grow well in the nervous system (
ref).
In any event, this reversion is problematic not so much for the vaccine recipient (who is well on the way to immunity) but for other residents of an area with poor sanitation. The transmission of vaccine strains to others in poor communities was originally held to be a feature, not a bug.
VAPP, which is extremely rare, finally became of crucial importance when polio was eliminated from most parts of the world. Then, having a risk of developing authentic polio out-weighed the advantage of the oral vaccine. When our son was born, we wrestled with the question of which vaccine to use for immunization. We chose Salk's IPV. Later, the vaccine schedule was changed to have the killed virus first and the live virus for boosters.
Here is a slide that shows the difference between IPV and OPV in the IgA response.
Although an IgA response is desirable, it is obviously not essential. IPV works well. That may well have something to do with the real pathogenesis happening in neural tissue.
Flu
The third vaccine to talk about is the live influenza vaccine. As a virus, influenza is unusual because it has a segmented genome, each gene is on a separate piece of RNA within the virus particle.
In epidemiology, influenza is different than most viruses because it mutates rapidly enough to escape the immune response within two or three years.
As with all viruses, a major component of the immune response is directed against proteins (antigens) on the surface of the virus. For influenza these are HA (hemagglutinin) and NA (neuraminidase).
HA (hemagglutinin) is a viral protein that binds to the receptors for influenza virus on animal cells. These receptors are proteins with sugar chains attached to them and with the special sugar
sialic acid attached at the end. HA binds to sialic acid. There are subtle differences in the structure of different forms of sialic acid between tissues or say, comparing human and avian hosts. Some HA bind better to human cells. HA is sometimes further abbreviated as H.
There is a second surface protein called NA (neuraminidase), further abbreviated N. Its role is to cleave sialic acid from the sugar chain when newly synthesized virus is leaving the cell. Different strains of influenza virus have different types of H and N.
The influenza virus from the 1918-20 pandemic, that has circulated in various permutations ever since, is H1N1. The virus of the 1956-57 pandemic was H2N2, and that for 1968-69 was H2N3.
This antigenic
drift means that a new vaccine must be formulated to best match the viruses that are circulating in any particular year. The segmented genome makes it fairly easy to produce a new vaccine strain by coinfecting cells with the virus whose HA and NA you want, plus the old vaccine strain. Reassortment of viral genome segments produces different combinations which can be screened to find the desired type that has attenuation mutations but the target HA and NA.
However, this also means that it is fairly easy (in evolutionary time) for completely new HA and NA genes to be transferred from avian flu strains to human flu strains. This is called antigenic
shift, and it happened successfully in 1918, 1956 and 1967. The 2009 virus came from pigs (although it must be noted that we gave it to them first, in 1918, so it's not really fair to complain).
Some more slides from one of my old lectures:
Other approaches
HPV (Human papilloma virus) comes in many serotypes. These viruses cause warts, but certain types are also associated with various cancers.
HPV is a small DNA virus and the proteins of the virus can self-assemble into a virus particle. One HPV vaccine is made from hollow "virus-like-particles" assembled from proteins made by recombinant DNA methods, without the genome inside.
There are other approaches to making vaccines that have the promise of more rapid scale-up including DNA and RNA vaccines, and recombinant proteins (e.g. the S or Spike protein). Also of importance are viruses that have been modified to not be harmful but can be used as carriers to express the desired cornavirus protein antigens. These include adenovirus and retrovirus-based vaccines.
For many of these, there is a concern that they will not boost the immune system as much as is necessary to give a good response. Various compounds (or even killed bacterial cells) act as adjuvants, treatments that increase the immune response. Many different combinations are possible and probably most of them are being tried.
It is noteworthy that the subunit vaccine (recombinant proteins) for pertussis (whooping cough) doesn't seem to be as active as the old vaccine, which had the drawback that most kids had soreness and redness at the site of the injection for several days.
Failures
We do not yet have successful vaccines for several important targets. These include HIV and malaria. In the case of HIV, the success of therapeutics may have something to do with the lack of progress on a vaccine, but it is a problem where many approaches have failed.
Risks
There are a couple of negative points to mention about vaccines.
One is that it is important to keep the vaccine formulation sterile. A tragic early event was the death of some Australian children due to injection with diphtheria vaccine that was contaminated with
Straphylococcus aureus (the Bundaberg disaster). The famous Australian scientist
Macfarlane Burnet had a role in solving this mystery.
A second issue is that occasionally, for a particular vaccine, the immune response makes an infection with the virus worse. The
example we have of this is a Dengue called Dengvaxia. However, this hasn't been seen with other viruses, or even other vaccines for Dengue.
Thimerosal
Finally, there is the issue of Thimerosal. After problems with vaccine preparations which had been stored and allowed bacterial growth, it became the practice to add low concentrations of a compound containing mercury called
thimerosal.
In the 1990s anti-vaccine activists popularized the notion that thimerosal in vaccines may have a connection to autism. In response, thimerosal was removed from vaccines for children by 2001. Rates of autism haven't changed, and there was never any evidence connecting thimerosal to autism. One prominent activist, Andrew Wakefield, was found guilty of scientific fraud. (He was motivated by payments by a group of lawyers who hoped to profit by suing vaccine manufacturers).
Non-human vaccines
There are a number of important vaccines for animals, including pets. The "core" vaccines recommended for all dogs are rabies, distemper, parvo, and adenovirus.